Interprofessional collaboration is recognised as an important factor in improving patient care. Interprofessional competency frameworks are increasingly being regarded as a key strategy to support the development of the requisite attitudes, knowledge, skills, and behaviours needed for the delivery of effective interprofessional care. However, evidence for the application of these competencies continues to remain limited in nature. To begin to fill this gap in the competency-based education literature, Goldman and colleagues undertook a study that aimed to investigate the implementation of interprofessional competencies in clinical practice.
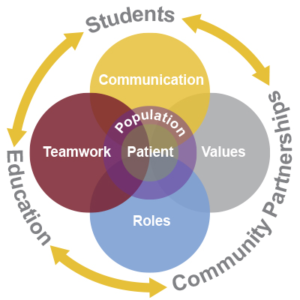
The study was undertaken in a medical surgical intensive care setting in a community teaching hospital in Canada. It employed an ethnographic approach to obtain in-depth insights into the perspectives, behaviours, and interactions of intensive care staff related to their collaborative practice. Around 160 hours of observations were undertaken and 24 semi-structured interviews with healthcare staff were conducted over a period of six months. Data were analysed using a directed content approach where two national North American competency frameworks (CIHC, 2010; IPEC 2011) – specifically the overlapping domains of interprofessional communication, role clarity, and team functioning – were used to help generate an understanding of the practice of interprofessional collaboration.
The results provided numerous instances where the competency domains of communication, role clarity, and teamwork were vital to the delivery of care. However, it was found that wider organisational factors (e.g. pressures for discharge and patient flow, adequate staffing levels, lack of prioritisation for interprofessional learning) made the enactment of such competencies problematic. For example, it was found that a hospital’s discharge policy, which placed pressure on the physicians for ‘timely discharges’ often resulted in them not engaging with other staff (e.g. nurses, pharmacists) around collaborative decision making – a core competency for effective team function (CIHC, 2010; IPEC 2011).
The findings from this study demonstrate that while interprofessional competencies play an important role in promoting collaborative knowledge, attitudes, skills, and behaviours needed for effective practice, the actual enactment of such competencies are dependent on a range of contextual factors (e.g. hospital policies) that can often impede their implementation. Given the nature of these findings, further research is needed to understand issues related to the enactment of competency frameworks, as this study suggests that many of the competences developed by educators fail to be implemented in clinical practice.
References
IPEC – Interprofessional Education Collaborative. (2011). Core competencies for interprofessional collaborative practice: Report of an expert panel. Retrieved from: http://www.aacp.org/resources/education/Documents/10-242IPECFullReportfinal.pdf
CIHC – Canadian Interprofessional Health Collaborative. (2010). A national interprofessional competency framework. Retrieved from http://www.cihc.ca/files/CIHC_IPCompetencies_Feb1210.pdf
To read more about this study
Goldman J, Kitto S & Reeves S (2017): Examining the implementation of collaborative competencies in a critical care setting: Key challenges for enacting competency-based education, Journal of Interprofessional Care, DOI: https://doi.org/10.1080/13561820.2017.1401987