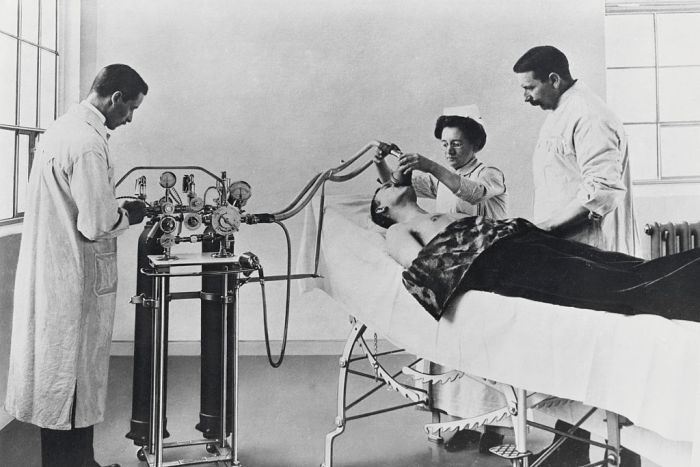
Photo: The discovery of general anaesthesia revolutionised medicine. (Getty Images: Bettmann)
Authors and affiliations at bottom of article
Introduction
Physician anesthesiologists and Certified Registered Nurse Anesthetists (CRNAs) have co-existed for over 100 years. The relationship between them has often not been the most collegial. This interprofessional conflict has manifested in situations in which the practice of CRNAs has been both legally challenged and restricted by their physician counterparts, frequently resulting in professional relationships that are not collaborative. To facilitate productive working relationships and positive patient outcomes, it is vital for nurse anesthetists and physician anesthesiologists to practice their respective professions collaboratively (AANA, 2012; Matsukai & Sakai, 2011). The Journal of Interprofessional Care (2016) defines interprofessional collaboration as a type of interprofessional work which involves different health and social care professions who regularly come together to provide services. Introducing collaborative practice must begin early in both professions, ideally when they are trainees (Alberto & Herth, 2009; AANA, 2013). The use of high-fidelity simulation involving both anesthesia residents and student nurse anesthetists is an important strategy for laying the groundwork for collaborative practice following transition into practice. High-fidelity simulation is an educational modality that allows the participants to engage in a clinically based simulation, in this situation, a learning laboratory that is designed as an operating room suite. The participants, when exposed to a high degree of realism, behave and act as they would if they were in a clinical situation working with patients and staff members rather than mannequins and confederates, often actors who portray clinical staff members ( Hinde, Gale, Anderson, Roberts & Sice, 2015;Matevski & Gravenstein, 2008; Palaganas, J.C., Epps, C., & Raemer, D.B., (2014).
Background
Anesthesia is unique in that anesthesia is administered by two primary types of providers, registered nurses, specifically CRNAs, and physician anesthesiologists, doctors of medicine or doctors of osteopathy. This frequently leads to interprofessional tension (AANA, Dillon, Noble & Kaplan, 2009). Whenever there is conflict between two professional providers, their working relationship may be compromised. Even more disconcerting is the possibility of a disruption in the teamwork required between the CRNA and the physician anesthesiologist ( AANA). Having two anesthesia providers concurrently delivering care often results in a practice overlap or a redundancy of services. (Dillon et al., 2009; Montgomery, Griswold-Theodorson, Morse, Montgomery & Farabough, 2012). Park, Spurr, and Chang (2009) stated that the scope of practice of both groups of providers is nearly identical, which may be a significant factor that contributes to interprofessional conflict. Interprofessional tension may develop from this overlap, which may have a negative impact on collaboration between CRNAs and physician anesthesiologists. Collaboration between both provider groups is essential since CRNAs and physician anesthesiologists use a team approach to deliver the majority of anesthetics, approximately 67% of cases ( AANA, 2012; Petri, 2009). Torgersen and Chamings (1994) explored collaborative relationships between physician anesthesiologists and CRNAs and concluded that poor collaboration resulted in negative working relationships and occupational stress, and compromised the delivery of quality anesthesia care (Petri, 2009). Conversely, positive collaborative relationships between CRNAs and physician anesthesiologists result in improved patient outcomes, and improved working relationships between these two groups of providers (Nagelhout & Plaus, 2014). Interprofessional collaboration is best served when there is mutual respect and communication among professionals, one strategy for promoting interprofessional collaboration is through interprofessional experiences using high-fidelity simulation (AANA, 2014, Palaganas et al., 2014).
Simulation in Anesthesiology
A viable strategy for interprofessional clinical training of student registered nurse anesthetists (SRNAs) and physician anesthesia residents is high-fidelity simulation (AANA, 2014; Matevski & Gravenstein, 2008). Interprofessional education through the use of high-fidelity simulation is a mechanism by which nurses and physicians may increase their understanding of their respective roles, improve communication and solidify a collaborative relationship that may have positive effects on the health care professional, the health care organization and the patient.
Traditionally, these two professional groups have been trained separately, and yet they are expected to work compatibly and collaboratively in the anesthesia care team (ACT) model, an anesthesia delivery model in which one anesthesiologist works with one to four CRNAs to provide anesthesia care in inpatient or outpatient settings (AANA, 2017; Dillon et al., 2009). When collaboration does occur in the work environment between nurse anesthetists and physician anesthesiologists, it is only after frequent exposure and validation of clinical expertise (Alberto & Herth, 2008; Matevski & Gravenstein, 2008; Dillon et al., 2009). Research has demonstrated that high-fidelity simulation among different health professions may promote more collaborative relationships (Alberto & Herth, 2008; Dillon et al., 2009; Hinde et al., 2016; Montgomery et al., 2012; Palaganas et al., 2014 & Petri, 2010). Therefore, it is logical that an interprofessional education experience provided through high-fidelity simulation during the training of anesthesia residents and SRNAs may be beneficial for promoting collaboration (Alberto & Herth, 2008; AANA, 2017). Scenarios in this form of simulated education can promote the identification of each providers’ strengths and weaknesses, may foster appropriate conflict resolution skills and promote an appreciation for each other’s individual and collective expertise (Alberto & Herth, 2008; AANA, 2017; Petri, 2010 & Park, Spur & Chang, 2009). Early and mutual learning opportunities for anesthesia providers has the potential to foster interprofessional teamwork and collaboration. Positive attitudes toward collaboration may also spread to the surgical suite and create a positive working environment for all members of the health care team.
Concluding comments
Interprofessional education through simulation may provide the opportunity for CRNAs and physician anesthesiologists to come together during their training to meet and work together in a safe, non-threatening environment. This experience may provide both providers with a basic introduction to each other’s skill sets and this exposure may also improve their ability to collaborate as professionals once their education is completed.
Authors and affiliations:
Michael E Conti
Nell Hodgins Woodruff School of Nursing, Emory University, USA
Email:mconti@emory.edu
Kelly L. Wiltse Nicely
Nell Hodgins Woodruff School of Nursing, Emory University, USA
Email: kelly.wiltse.nicely@emory.edu
References
AANA Product Media Planner (2012). Retrieved from: http://www.aana.com/newsandjournal/Documents/2012product-media-planner.pdf
AANA State Government Affairs Fact Sheet (2013). Retrieved from: http://www.aana.com/advocacy/stategovernmentaffairs/Pages/Fact-Sheet-Concernintate-Opt-Outs.aspx
AANA.com (2017) Retrieved from http://www.aana.com/ceandeducation/becomeacrna/Pages/Nurse-Anesthetists-at-a-Glance.aspx
Alberto, J. & Herth, K. (2009) Interprofessional collaboration within faculty roles: Teaching, service and research. The Online Journal of Issues in Nursing. (14) 2.
Dillon, P.M., Noble, K., & Kaplan, L. (2009) Simulation as a means to foster collaborative interdisciplinary education. Nursing Education Research. (30)2: 87-90.
Hinde, T., Gale, T., Anderson, I.,Roberts, M., & Sice, P. (2016). A study to assess the influence of interprofessional point of care simulation training on safety culture in the operating theatre environment of a university teaching hospital. The Journal of Interprofessional Care. (30)2: 251-253.
The Journal of Interprofessional Care (2017) Retrieved from http://www.tandfonline.com/action/authorSubmission?show=instructions&journalCode=ijic20
Matsuskai, T. & Sakai, T. (2011). The role of the nurse anesthetists in the United States. Journal of Anesthesiology. 25: 734-740.
Matevski, A.S. & Gravenstein, N. (2008). Role of simulators, educational programs, and non-technical skills in anesthesia resident selection, education and competency assessment. Journal of Critical Care. (23):167-172.
Montgomery, K., Griswold-Theodorson, S., Morse, K., Montgomery, O. & Farabaugh, D. (2012). Transdisciplinary simulation: Learning and practicing together. Nursing Clinics of North America. Philadelphia: Elsevier Press.
Naglehout, J.J. & Plaus, K.L. Nurse Anesthesia. 2014 St. Louis: Saunders Elsevier.
Palaganas, J.C., Epps, C., & Raemer, D.B. (2014). A history of simulation-enhanced interprofessional education. The Journal of Interprofessional Care. (28)2: 110-115.
Park, J-H, Spurr, S.J., & Chang, S-K. (2009). A model of hierarchical professionals: Cooperation and conflict between anesthesiologists and CRNAs. Center for Economic Institutions, Hitosubashi University, Tokyo.
Petri, L. (2010). Concept analysis of interdisciplinary collaboration. Nursing Forum: 2010; (45) 2:73-82.